Is Minimally Invasive Lumbar Discectomy better than Open?
Is Minimally Invasive Lumbar Discectomy better than Open?
Inter-vertebral disc herniation in the lumbar spine is a common clinical condition. It accounts for 5% of lower back disorders and is the commonest reason for low back surgery. Patients commonly present with pain radiating from buttocks to a leg below the knee (sciatica) due to compression or irritation on nerve roots supplying the lower limbs by the herniated disc fragment. Majority of patients respond well to a period of conservative treatment including physiotherapy and anti-inflammatory medications. Surgery is indicated for patients who failed after a period of conservative treatment and for those with significant neurological deficits.
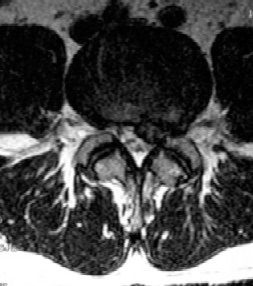
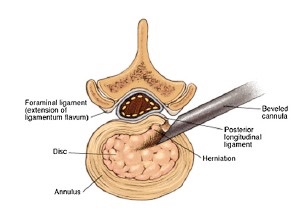
Traditionally the surgery is done with open surgery. The procedure is done via a mid-line posterior longitudinal skin wound over the herniated lumbar disc segment. The posterior parts of the vertebrae (laminae) are exposed with sub-periosteal dissection. A window is made at the laminae (laminotomy) and the herniated part of the inter-vertebral disc is then removed (discectomy). Good to excellent results can be achieved in 60 to 90% of patients.
Minimally invasive lumbar discectomies are getting popular in recent few years. They can be classified to two main group: microendoscopic diskectomy (MED) and percutaneous endoscopic lumbar diskectomy (PELD).
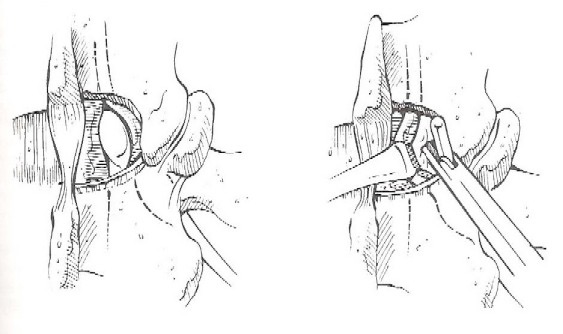
Micro-endoscopic discectomy is performed by means of a para-spinal muscle splitting approach with tubular dilators and retractors, laminotomy and discectomy are subsequently performed under microscopic guidance.
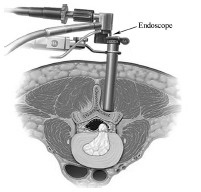
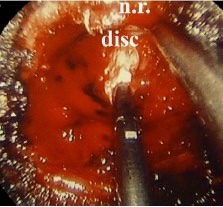
Percutaneous endoscopic discectomy is performed with an endoscope inserted percutaneously, commonly via transforaminal approach to the herniated disk fragment, diskectomy is subsequently done under endoscopic guidance.

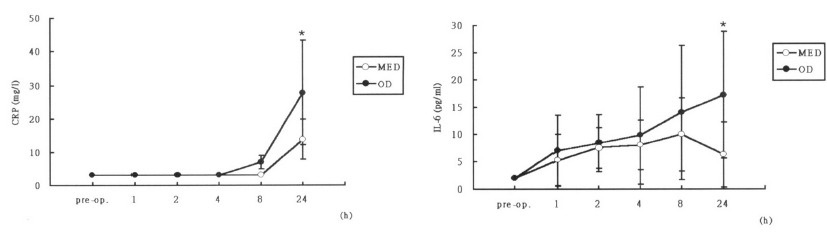
People advocating minimally invasive techniques commonly claim that they cause less surgical trauma to patients with less post-operative inflammatory response. However, whether they can really produce better clinical outcomes is still uncertain. Randomized controlled studies comparing minimally invasive lumbar discectomy with open discectomy so far available are of low quality. They are not blinded studies and are of small sample sizes. MED and PELD had smaller surgical wounds, ranging from 0.5cm to 4.4 cm and less wound pain at the early post-operative period compared with open discectomy. However, there is no difference in medium and long term follow up.
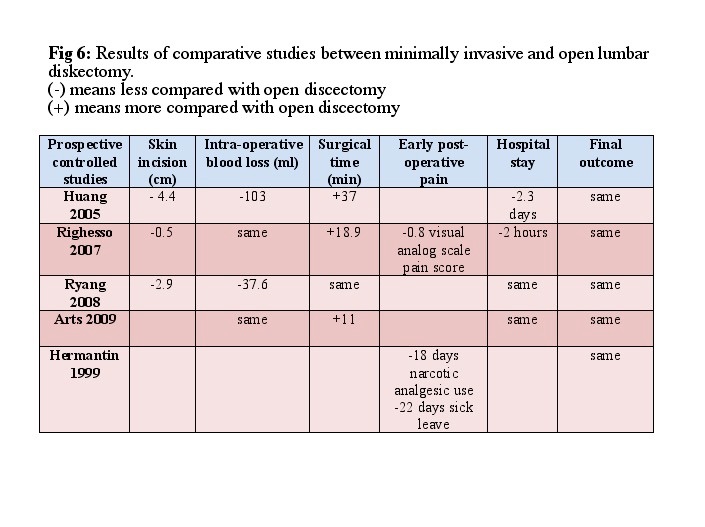
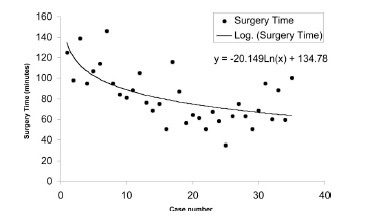
Special surgical instruments are required for minimally invasive techniques and the learning curve for the surgeon is steep. Duration of surgery may be up to 2 times that of normal and surgical complication rate up to 20% has been reported even under the hands of experienced surgeons.
Whether minimally invasive lumbar diskectomy is better than open is surgeon dependent. In experienced hands, the surgical wounds are smaller and there is less pain in the early post-operative period.
Dr. CHEUNG, Wai-yuen