Introduction
Causes of bone defect
Types of bone graft and bone substitutes
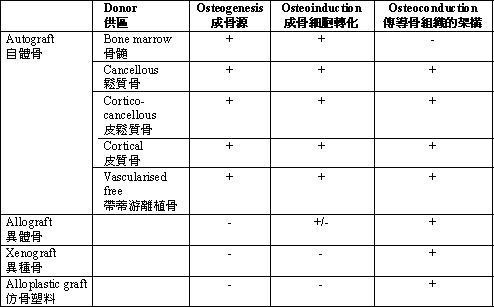
The properties of common bone grafts or bone substitutes are tabulated:
Introduction
The use of bone grafts in Orthopaedic Surgery is very common. The most common indication is to fill up of any bony deficiency.
Less common indications are:
1. To act as a structural support for skeletal integrity
2. To stimulate bone formation from the host bone: as a structural scaffold or as a bone growth stimulant
3. To facilitate bony union, say in repairing fractures or in fusion of mobile skeletal segments, arthrodesis or spinal segment fusion
4. To stabilize an implant e.g. as impaction bone graft in revision of loosen joint components
Recently various types of bone substitutes have been applied instead of traditional bone grafts. Custom-made prosthesis are the other alternative when a patient has a large bone defect or when a patient has had bone tumour surgery or revision joint reconstruction.
Causes of bone defect
Bone substance may be lost due to congenital absence, injury or destruction by pathologies such as infection, neoplasm or inflammatory diseases. Unlike many other tissues, bone can grow and may even regenerate completely under suitable circumstances. Bone grafts or bone substitutes are used because they provide a good environment for the bone to replenish the defect, whatever the cause.
Types of bone graft and bone substitutes
Autograft – when bone is obtained from the individual that is receiving the graft. Iliac crest (on the edge of the pelvis) and the fibula are both common sites for harvesting autografts. Both are effective at treating bone defects but post-operative pain or other complications at the donor site can be experienced. Depending on the circumstance, different parts of the bone can also be applied as autografts:
Cancellous – good for its bone forming potential.
Cortical – good for providing mechanical support especially before new bone is well formed.
Cortico-cancellous – combines the merits of both cancellous and cortical bone.
Vascularised free graft – where bone with nutrient artery and veins are also harvested. If the recipient site is far away, the nutrient artery and veins will be divided and then re-anastomosed to the artery and veins at the recipient site using microsurgical technique. For recipient sites that are nearby, the bone may be moved to the desired position without dividing its vascular pedicle, the pedicled bone graft.
Bone marrow injection – it stimulates bone growth because it contains growth factors and cells that may be developed into bone-forming cells. There is no mechanical strength and this has to be used in combination with other methods.
Allograft – human bone harvested from an individual other than the recipient. Bone may be harvested from donors after their deaths (cadaveric donors) or sometimes from life donors when bone has to be removed from patients in the process of treating a certain problem. A common example is in the case of fracture at the neck of the femur. The affected femoral head would have to be removed and replaced with a metallic prosthesis. The femoral head removed will be discarded even if it is not harvested into the bone bank.
Allografts can be prepared by the following methods:
Fresh frozen bone - This is the most common form of allograft used in Hong Kong. To prevent the transmission of diseases and to prevent organ trading, strict measures are required for the harvesting and use of allograft. The bone harvested is stored in a bone bank until the possibility of transmissable diseases is excluded by stringent tests. Only allografts that have passed the tests can be put into clinical use.
Freeze-dried bone allograft and Demineralised freeze-dried bone allograft processes are also sometimes used.
Xenograft – bone obtained from a species other than human, usually from bovine bone.
Alloplastic graft – bone graft made from synthetic material. Calcium carbonate was used in the early days. It is completely resorbed after a short period of time and the resulting bone may fracture before it is fully consolidated. This is being replaced by ceramics and denser materials such as calcium triphosphate and hydroxyapatite.
Growth factors – bone morphogenic proteins (BMPs) can stimulate the growth of bone-forming cells (osteoblasts) and is produced using recombinant DNA technology. About 20 BMPs has been discovered. Of these, BMP2 and BMP7 are currently commercially available.
Bone forming cells known as osteoblasts are required for bone growth. Osteoblasts and their precursor cells are present in normal bone and they are stimulated to produce bone by growth factors. There are 3 mechanisms underlying the use of bone grafts:
Osteogenesis – osteoblasts from the donor bone survive and contribute towards the growth of new bone.
Osteoinduction – the ability to stimulate formation of new osteoblasts from precursor cells in vicinity. Bone morphogenic proteins are the most widely studied osteoinductive mediator.
Osteoconduction – The ability to provide a scaffold for the new bone to grow into. Bone is being formed by the native osteoblasts near the bone defect.
The properties of common bone grafts or bone substitutes are tabulated:
Dr. YEUNG, Sai-hung