Anatomy
Cause
Symptoms
Diagnosis
Non-surgical treatment
Surgical treatment
Prevention
Anatomy
The term osteoporosis literally means porous bone.
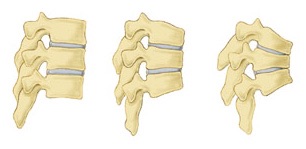
Our skeleton is made up of a spinal column supporting the limb girdles, the shoulder and the pelvis. To maintain an erect posture, the weight of the trunk and the load that it carries has to be taken up by the lower limbs and the pelvis. If the bone has become porous, it is not strong enough to sustain the stress from weight-bearing, and fatigue fractures may develop. Such fractures may not be obvious apart from some pain. The more porous the bone is, the more likely it fractures without having undergone significant trauma.
Cause
Doctors do not know the exact medical causes of osteoporosis, but they have identified many of the major factors that can lead to the disease.
Aging: Everyone loses bone with age. After 35 years of age, the body builds less new bone to replace the loss of old bone. In general, the older a person is, the lower the total bone mass and the greater the risk for osteoporosis.
Heredity: A family history of fractures; a small, slender body build; fair skin; and Caucasian or Asian ethnicity can increase the risk for osteoporosis. Heredity also may help explain why some people develop osteoporosis early in life.
Nutrition and lifestyle: Poor nutrition, including a low calcium diet, low body weight and a sedentary lifestyle have been linked to osteoporosis, as have smoking and excessive alcohol use.
Medications and other illnesses: Osteoporosis has been linked to the use of some medications, including steroids, and to other illnesses, including some thyroid problems.
Symptoms
The disease often develops unnoticed over many years, with no symptoms or discomfort until a fracture occurs. Osteoporosis often causes a loss of height and a severely rounded upper back. This is the result of a partial collapse of a weakened vertebrae.
Diagnosis
The diagnosis of osteoporosis is usually made by your doctor using a combination of a complete medical history and physical examination, skeletal X-rays, bone densitometry and specialised laboratory tests. If your doctor diagnoses low bone mass, he or she may want to perform additional tests to rule out the possibility of other diseases that can cause bone loss, including osteomalacia or hyperparathyroidism.
Non-surgical treatment
Because lost bone cannot be replaced, treatment for osteoporosis focuses on the prevention of further bone loss. Treatment is often a team effort involving a physician or internist, an orthopaedist, a gynecologist and an endocrinologist.
Although exercise and nutrition therapy are often key components of a treatment plan for osteoporosis, there are other treatments as well.
Estrogen Replacement Therapy (ERT): often recommended for women at high risk for osteoporosis to prevent bone loss and reduce fracture risk. A measurement of bone density when menopause begins can help decide if ERT is the right treatment. Some ERT-related risks include breast cancer; but the risks and benefits should be discussed with your doctor.
Selective Estrogen Receptor Modulators (SERMs): new anti-estrogens known as SERMs can increase bone mass, decrease the risk of spine fractures and lower the risk of breast cancer.
Calcitonin: another medication used to decrease bone loss. A nasal spray form of this medication increases bone mass, limits spine fractures and may offer some pain relief.
Bisphosphonates: a type of medication that markedly increases bone mass and prevent both spine and hip fractures.
ERT, SERMs, calcitonin and bisphosphonates all offer patients with osteoporosis an opportunity to not only increase bone mass, but to also significantly reduce the risk of fractures. Prevention is preferable to waiting until treatment is necessary.
Surgical treatment
Surgical treatment of osteoporotic spinal fractures is usually not necessary, unless there are neurological complications due to the degeneration of the spinal canal. If there is a narrowing of the spinal canal as a result of a fracture, kyphosis (angular deformity of the spine) or displaced vertebral structures, surgical decompression might be necessary to relieve the affected neural tissues.
There are also procedures to correct the collapsed vertebral body by means of a cement injection (known as a “filler”). The filler is injected into the spine directly by using a needle in a close surgery. The filler commonly used today is orthopaedic bone cement, which hardens in about 10 minutes after preparation. It might be able to restore the height of a collapsed vertebral body and hence correct the angular deformity (kyphosis) of the spine. Since the procedure does not involve open surgery, it takes only about two hours.
A new type of filler is Strontium, a naturally occurring, metallic chemical element. After injection, the element acts as a kind of “bone cement” to strengthen the bone structure.
Prevention
Calcium: During the growing years, your body needs calcium to build strong bones and to create a supply of calcium reserves. Inadequate calcium during growth can contribute to the development of osteoporosis later in life. Calcium continues to be an essential nutrient after growth because the body loses calcium every day. Although calcium cannot prevent gradual bone loss after menopause, it continues to play an essential role in maintaining bone quality. Even if women have gone through menopause or already have osteoporosis, increasing the intake of calcium and vitamin D can decrease the risk of fracture.
Vitamin D: Vitamin D helps your body absorb calcium. The recommendation for vitamin D is 200-600 IU (international units) daily.
Exercise regularly: Exercise can help minimise bone loss while providing many additional health benefits. Doctors believe that a programme of moderate, regular exercise (3 to 4 times a week) is effective for the prevention and management of osteoporosis. Weight-bearing exercises such as walking, jogging, hiking, climbing stairs, dancing, treadmill exercises and weight lifting are probably best. Falls account for 50% of fractures; therefore, even if you have low bone density, you can prevent fractures if you avoid falls. Programmes that emphasise balance training, especially tai chi, are highly recommended.