Bow Leg and Knock Knee
Bow Leg and Knock Knee
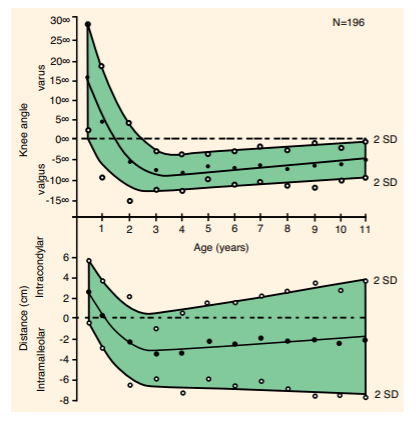
Baby is born with bow leg, an outward curvature of knee and lower leg. The knee angle (the angle between the tibia and femur) at birth is normally about 10-15∘. The knee ankle increases with age, becomes maximal at age of 6 month. The bow legs can appear quite impressive when the baby starts to stand or walk because they tends to walk with their hips external rotated with the plane of knee flexion in external rotation. With their knees flexed during walking, the knee separate. The bow leg then straightens out by the age of 18 months or 2 years. It then grows into mild knock knee by the age of 2 to 3. The knock knee becomes peak at age of 4, at that time the knee angle can be 10-12∘. It then gradually straightens out thereafter. By the age of 7, the knee looks similar to that of adult, a slight appearance of knock knee of 5-6∘. Such changes may be quantified by the knee angle or the distance between the ankle medial malleolus (intra-malleolar distance) or the distance between the knee medial condyle (intra-condylar distance). The graph below shows the mean and 95th percentile of the knee angle and intermalleolar or intercondylar distance with age in 196 normal children aged 6 months to 11 years (CH Heath & LT Stehali 1993). A large scale study of 1,480 children on radiographic knee angle showed the same trend. It should be noted that the normal range is wide, as indicated by a standard deviation of 8∘.
The physiological bow leg or knock knee is symmetrical, without symptoms, no pain, no joint stiffness. These are examples of normal growth variations, which are common and resolve with growth. Observe the child, give them time. No treatment is necessary. Special shoes, wedges, inserts or exercises only make the child feel bad and do not correct the shape.
Pathological bow leg is due to a disease process and will get worse with time if not treated. We should be concerned and seek medical treatment if the bow leg is not resolved by age of 3; the bowing is severe, unilateral or asymmetrical; the bowing is associated with pain, short stature (especially runs in family) or poor nutrition. Blount’s disease is rare in Chinese but rickets may occur in Hong Kong, particularly among the ethnic minorities.
The majority of knock knees are normal variance. Some knock knees may be pathological due to a number of causes. Common examples are fracture malunion or injury to physeal growth plate around the knee. Less common causes include skeletal dysplasia and metabolic bone disease such as nutritional rickets in early adolescents. Similarly, if the knock knee is asymmetrical or unilateral; too severe (the knee angle > 12∘ or the intermalleolar distance > 8 cm); persistence by the age of 8, progressive deformity in older age, medical treatment should be sought.
In skeletal immature children, angular deformity of knee may be corrected surgically by temporary hemiepiphysiodesis. A device (eight-plate or staple) is positioned to slow or stop the bone growth on one side of the growth plate. The other side of the growth plate continues to grow normally. This will gradually straighten the knee in 6 to 12 months or longer. The hardware is removed when full correction of the deformity, or slight overcorrection to account for some expected rebound) is obtained. The entire physis resumes growth after hardware removal. Modulating growth by hemiepiphysiodesis is a gentle, less invasive and effective alternative to corrective osteotomy; guided growth has advantages of less pain, shorter immobilization and less surgical risk.
In skeletal mature adolescents, corrective osteotomy is required to correct the deformity. Here is an example of asymmetrical genu valgum in a 13-year-old girl. The tibiofemoral angle on the right side was 25∘with an inter-malleolar distance of 23 cm. Corrective osteotomy of distal femur and proximal tibia restore the symmetrical alignment of lower limbs. Blood investigation showed nutritional rickets from vitamin D deficiency.
Dr Ho Sheung Tung
 before operation
before operation
 after correction
after correction
 before operation
before operation
 after correction
after correction